The Effect of Osteopathic Treatment For People with Chronic and Sub-Chronic Neck Pain. Summary and Critical Analysis.
- by Joanna Blair
- •
- 02 Oct, 2017
- •

- The following study investigated whether one month's protocol of osteopathic treatment could be effective for subjects complaining of intermittent or constant neck pain.
- Subjects received six treatment sessions which were performed via fifth year osteopathic students under the supervision of a qualified, registered osteopath.
- Overall, results for this *pilot study concluded that Osteopathic treatment may be effective for the management of sub-chronic and chronic neck pain and help significantly reduce the quality and intensity of neck pain over a 4-week treatment period.
- It was found that future research using a larger sample size, a control
group, and a longer period to monitor the long-term
improvement is recommended.
Aim
The aim of the pilot study was to examine the effect of osteopathic management for people with neck pain.
Neck Pain Background Information
Neck pain is a common problem and it is estimated that two thirds of the general population will suffer with neck pain at some point within their lifetime (1.). Patients often complain of limited range of motion and stiffness which can be precipitated or aggravated by neck movements or maintained neck postures. Headache, brachialgia (pain in the brachium of the arm) and dizziness can also be symptoms with neck pain (2.).
Sub-Chronic Neck Pain
Constant pain for 5-7 weeks but no longer than 12 weeks (3.).
Chronic Neck Pain
Pain present for at least 3 months since onset or suffering with continuous pain for more than a 12 month period (3.).
Aetiology of Neck Pain Related To Trauma:
Bogduk and Yoganandan (2001) studied biomechanics of minor and major whiplash injuries and concluded that compressive forces were the more likely cause to injury and mainly produce impact within the lower cervical zygapophysial joints (4.).
Non-Traumatic Aetiology of Neck Pain
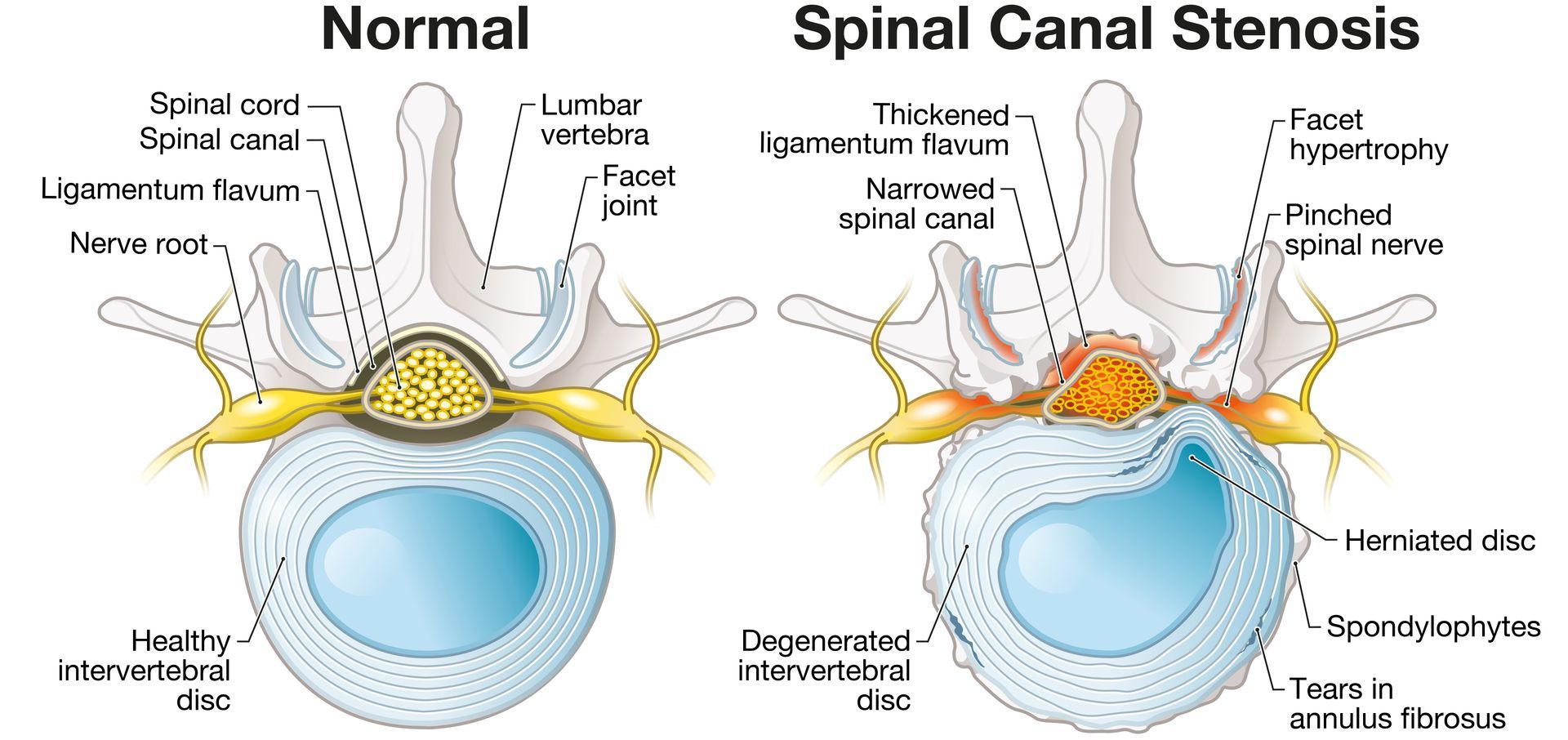
The aetiology of non-traumatic neck pain is less clear, and may involve the cervical intervertebral discs and zygapophysial joints, as is commonly the case in lower back pain (5.). Additionally, chronic neck pain may involve neuroplastic changes in the dorsal horn of the spinal cord and the sensitisation of nociceptive pathways (6.).
Osteopathic Treatment to the Cervical Spine
Osteopathic treatment often consists of a combination of manual techniques, including high velocity, low amplitude thrust (HVLA) osteopathic spinal manipulation, soft tissue technique, passive mobilisation (articulation), functional (indirect) technique, myofascial release, craniosacral therapy and muscle energy technique.
Study Method
Overall, 13 subjects were enrolled and completed the pilot study. Twenty one subjects were initially recruited and were either students from Victoria University in Australia or from businesses in the Melbourne Central business district.
Four subjects attended the initial visit but did not attend for further treatment or complete post treatment questionnaires and were excluded
from the study which left seventeen subjects. Another four subjects in the study
were not present at week 4 to complete the final post treatment questionnaire.
Subject Recruitment
- Subjects were redeemed adequate if they suffered from intermittent or constant neck pain for a duration longer than 1 month.
- Individuals were excluded if they had suffered constant unremitting neck pain for greater than
12 months, had any neurological signs or symptoms, or had a history of cervical
intervertebral disc prolapse or trauma such as whiplash.
- The
study was divided into sub-groups: ‘sub-chronic’ = symptoms less than 12 months duration and ‘chronic’ = symptoms lasting greater than 12 months to analyse whether the duration of symptoms influenced neck pain recovery.
- The mean age of the subjects of the cohort group was 34.8 years old, the mean duration of symptoms was 168.8 weeks (or over 3 years) and the duration range of symptoms was between 4 to 1040 weeks (twenty years).
- The cohort group was divided into two sub-groups to examine the duration of symptoms on recovery into a ‘sub-chronic’ group where the duration of symptoms was less than 52 weeks and the ‘chronic’ group where symptoms lasted more than 52 weeks.
- The mean age of the sub-chronic group was 33.6 years, the gender ratio was 1:1 and the mean duration of symptoms was 23.8 weeks (or more than 3 weeks).
- The mean age of the chronic group was 36.5 years and the mean duration of symptoms was 376 weeks and included 5-female and 2-male subjects.
- Four subjects did not return for treatment to complete the questionnaires at week 4 for the McGill pain questionnaire
Outcome Measures
Treatment outcomes were measured using:
1.) The McGill pain questionnaire (MPQ).
- Used to evaluate a person experiencing significant pain and used to monitor pain over time to determine the effectiveness of any intervention.
- Analyses three separate components of the experience of pain; (i.) sensation (ii.) the emotional effect and (iii.) the cognitive assessment of the individual.
- Subjects were presented with 80 adjectives and had to select one from each group that best describes their own pain. The words are given a numerical scale rating from ‘mildest’ to ‘worst’, and the sum of these scores represents the total Pain Rating Index (PRI). Present pain intensity (PPI) is also determined with a scale ratio from 0 to 5
2.) 100 mm visual analogue scale (VAS).
- Psychometric response scales used to measure subjective characteristics or attitudes scored between 1 and 100mm (Klimek et al.,
2017).
3.) The neck disability index (NDI) questionnaire (an otherwise modified questionnaire version of the Oswestry Low Back Pain Index).
- A 10-item scaled questionnaire each with a score of up to 5 ('points') for a total of 50. The lower the score, the less self-rated disability.
Questionnaires asked certain aspects of disability such as pain, including headaches and the ability to perform tasks like personal care, lifting, reading, driving and recreation. Subjects chose the statement that best described their situation in each section of the questionnaires.
Method
- Subjects were offered a 4-week course of osteopathic
treatment at the Victoria University Osteopathic Medicine Clinic (OMC), Australia.
- Individuals were requested to fill out the three questionnaires; MPQ, VAS and NDI to indicate their perceived pain and disability before the initial consultation and after the treatment sessions at weeks 2 and 4.
- The four practitioners performing treatments were fifth year (senior) osteopathic students and under the supervision of a registered osteopath. Subjects who underwent cervical HVLA were screened for vertebral artery insufficiency (VBI).
- A semi-standardised treatment protocol was used by the four practitioners to provide consistency for each patient and could be varied at the discretion of the practitioners clinical findings.
- The chosen treatment techniques were selected as they described standard osteopathic texts and the researchers believed they are commonly used by osteopathic practitioners to treat neck pain.
1. Soft tissue technique (cross-fibre kneading, inhibition) to trapezius, cervical, thoracic erector spinae, levator scapulae, and sub-occipital muscles.
2. Articulation (passive joint mobilisation) to the cervical and thoracic spine.
3. Muscle energy technique (isometric facilitated stretching) to the scalenes, levator scapulae, trapezius, sternocleidomastoid muscles.
4. Counterstrain technique (positional release) at the discretion of the practitioner. HVLA to the cervical or thoracic vertebrae at the discretion of the practitioner.
- All subjects received the first 3 treatment
procedures, the 4th and 5th techniques were used at the discretion
of the treating practitioner. The treatment of other areas was also performed if the practitioner felt it necessary e.g.the treatment of the pelvis or lumbar spine.
- Subjects were offered postural advice and exercise prescription (neck mobility and
stretching) at the discretion of the practitioner.
- Subjects were requested to undertake osteopathic treatment twice a week for 2 weeks, and once a week for a further 2 weeks (overall 6 osteopathy treatments were performed).
- Subjects were
requested to complete the questionnaires prior to the initial treatment and
then after treatment at weeks 2 and 4. After the completion of the trial
period, the scores from the questionnaires were analysed and compared for pre and post treatment differences.
Study Results
- Both the subchronic and chronic sub-groups had a reduction in mean scores from pre-treatment to 2 weeks and to 4 weeks.
- Overall, the results showed significant reductions in pain intensity (VAS), pain quality (MPQ) and disability (NDI) throughout the study trial.
- There was a large reduction in mean scores over time from pretreatment to 2 weeks and to 4 weeks and the repeated measures ANOVA test found significant differences over time.
- Analysis of the sub-group MPQ scores showed that there were significant differences between time groups for both the sub-chronic and chronic groups.
- Further analysis using paired t-tests revealed the differences in mean scores between pre-treatment and 4 weeks and between 2 and 4 weeks for both sub-groups, but no significant difference was seen between pre-treatment and 2 weeks.
- A large pre/post treatment effect size (pre-treatmente to 4 weeks) was noted for the MPQ for the sub-chronic group. A medium to large effect size was found for the chronic group.
- The mean VAS scores for the cohort group reduced over time, from pre-treatment to 2 weeks and 4 weeks.
- The sub-groups showed similar trends, with the sub-chronic group having a reduction in pain -from pre-treatment to 2 weeks and post-4 weeks, and the chronic group with a reduction from pre-treatment to 2 weeks and 4 weeks.
- Significant differences were revealed over time and further analysis with paired t-tests showed the differences to be between pre-treatment and 2 weeks and between pre-treatment and 4 weeks. No significant difference was seen between the scores at 2 and 4 weeks. There was a large pre/post (pre-treatment 4 weeks) effect size for the VAS in the cohort group.
- This study demonstrated that osteopathic treatment significantly reduced neck pain in a cohort of individuals suffering from sub-chronic and chronic neck complaints.
- Neck disability index scores for the cohort group showed an overall decrease in mean scores from pre-treatment to week 2 and week 4. Further analysis using paired t-tests showed the differences to be between pre-treatment and 2 weeks, pre-treatment and 4 weeks and between 2 and 4 weeks.
- Further analysis using paired t-tests showed the differences to be between pretreatment and post-2 weeks and between pre-treatment and post-4 weeks for both sub-groups.
- Large pre/post (pre-treatment 4 weeks) effect sizes were observed for the NDI in both the sub-chronic and chronic groups.
Discussion and Short Critical Analysis:
Short Summary of Overall Results
- The cohort group was subdivided into those who had suffered with neck pain for less than one year (sub-chronic) or greater than one year (chronic) and both groups showed similar significant changes over the course of treatment.
- Osteopathic treatment was found to significantly decrease the quality and intensity of neck pain over a 4-week treatment period.
- Significant reductions were found in pain intensity, pain quality and disability when comparing pre-treatment with 2-week measures and pre-treatment with 4-week measures for both sub-groups.
- The mean scores for all three measures decreased over each time period for both sub-groups, but there was no statistically significant change for the MPQ between pre-treatment and 2 weeks, or for the VAS or NDI between weeks 2 and 4.
- The results showed that the majority of subjects may have experienced periods of reduced pain during the course of treatment, but most did not experience a full resolution.
- In the present study, no significant reduction of the PPI over time was found, whereas there was a highly significant reduction in the VAS, as well as in the other outcome measures.
- A methodical treatment approach was used for this study rather than a treatment left totally to the discretion of the practitioner. Osteopathic manipulative approaches can vary between practitioners and the authors of the study believed it was important to maintain some consistency for each treatment.
- The treatment techniques selected for the study were chosen because they were described in standard osteopathic texts and the researchers believed they are commonly used by osteopathic practitioners to treat neck pain.
- The treatments were largely constrained to ‘structural’ or ‘direct’ approaches, rather than indirect methods such as functional and ‘balanced ligamentous tension’ techniques.
- There was a certain degree of flexibility within the treatment protocol. Tthere were no time limits on application of any technique, and the use of more specific techniques (such as HVLA and counterstrain) and treatment of more remote regions (such as the lumbar spine and pelvis) were entirely at the discretion of the treating osteopath.
Placebo /Control Group
- The study examined a single cohort, and did not include a control group (using either no treatment or standard medical care)due to budget and practical constraints.
- There is a possibility that the improvements found from patients was as a result of placebo or the natural course of the complaint.
- Even if the issue of an absent placebo group contributes significantly to the changes in outcome measures, the fact remains that these individuals appeared to receive substantial improvement in their pain and disability after having received osteopathic treatment.
- A control group would have been a useful addition to future studies to compare the effect of the natural course of the condition.
- This study examined the effect of osteopathic management over the course of a 4-week treatment programme, but did not track the improvement in outcomes over a longer period of time. The lasting benefit of treatment to these subjects is unknown as a result.
- Future studies should examine the effect of osteopathic management over a longer time frame to establish the longevity of benefit of treatment and the optimal frequency of osteopathic manipulation needed to maintain these benefits.
Study Size
- Future studies need to include a larger sample size, have an adequate longer-term assessment.
- Compare osteopathic management with other treatment modalities such as physiotherapy or exercise prescription.
References
1. Cote, P., Cassidy, J. D., Carroll, L. (1998) The Saskatchewan Health and Back Pain Survey: the Prevalence of Neck Pain and Related Disability in Saskatchewan Adults. Spine; 23: 1689–98.
2. Anderson, H. I., Ejlertsson, G., Leden, I., Rosenburg, C. (1993) Chronic Pain in a Geographically Defined General Population: Studies of Differences in Age, Gender, Social Class and Pain Localisation. Clin J Pain; 9 : 174–82.
3. Merskey, H., Bogduk, N. (1994) Classification of Chronic Pain. Description of Chronic Pain Syndromes and Definitions of Pain Terms, 2nd Ed. Seattle, IASP Press.
4. Bogduk, N., Yoganandan, N. (2001) Biomechanics of the cervical spine part 3: minor injuries. Clin Biomech; 16: 267–75.
5. Bogduk, N. (1997) Clinical anatomy of the lumbar spine and sacrum. 3rd ed. Churchill Livingstone.
6. Curatolo, M., Arendt-Nielsen, L., Petersen-Felix, S. (2004) Evidence, Mechanisms, and Clinical Implications of Central Hypersensitivity in Chronic Pain After Whiplash Injury. Clin J Pain; 20:469–76.